Neuroscience

Most of us have had frightening nightmares – someone is chasing after us trying to kill us, or the world is coming to an end. Other disturbing dreams are based on real life anxieties – our partner leaves us, we lose our job, we become homeless. One specific psychiatric condition includes nightmares as part of the diagnosis. Individuals with post-traumatic stress disorder (PTSD) often have terrible nightmares that relive the traumatic event (Pigeon et al., 2013)
We're always glad to wake up from such nightmares, whether they were of the supernatural or mundane or terrifying variety. "Thank god it was only a dream," we say.
But what if waking up from sleep was the nightmare? Hypnopompic hallucinations are unusual sensory phenomena experienced just before or during awakening. Their better known mirror image, hypnagogic hallucinations, are vivid and frightening episodes of seeing or hearing or feeling phantom sensations while falling asleep (or in early stage 1 sleep). Both are frequently associated with sleep paralysis, the terrifying condition of being half awake but unable to move. This is because the complete muscle atonia typically experienced during REM sleep has oozed into lighter stages of non-REM sleep.

Hypnagogic and hypnopompic hallucinations are usually associated with narcolepsy, but 37% of a representative community sample reported frequent hypnagogic hallucinations, and 12.5% reported hypnopompic hallucinations (Ohayon et al., 1996).1 This went well beyond the low incidence of narcolepsy in that population. Both types of hallucinations were more common in those with insomnia, excessive daytime sleepiness, anxiety disorders, and depression (according to self-report).

Nocturnal Episodes of Pain and Screaming
A new case study in the journal Sleep (Mantoan et al., 2013) reports on the terrifying hypnopompic hallucinations of a 43 year old woman who experiences intense limb pain when waking up, which vanishes within 30 seconds. This is a very unusual manifestation of a non-REM parasomnia, a sleep disorder involving partial arousal during the transition between non-REM and wakefulness. The phenomenology might be best characterized as a night terror.
According to the case report (Mantoan et al., 2013), the patient had...
She initially had these episodes monthly, but they increased in frequency to 2-5 times a week with 1-2 episodes per night.
The authors could not identify any standard physical source for the pain. Thoracic outlet syndrome, cervical radiculopathy, focal nerve entrapment, and median neuropathy (carpal tunnel syndrome) were all ruled out.
Pharmacological treatments were unsuccessful. A low dose (0.5–1 mg) of clonazepam was poorly tolerated (it made her feel depressed) and had no effect on her symptoms. Paroxetine was poorly tolerated (due to sedative effects), and gabapentin was also a complete failure. Trazodone, a sedating antidepressant most often prescribed for insomnia, actually made the symptoms worse.
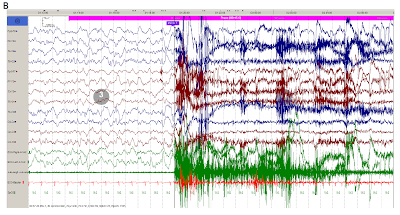
An MRI ruled out a thalamic or hypothalamic lesion. Sleep EEG revealed sudden arousals from deep sleep, accompanied by looks of pain and/or fear on the patient's face. The episodes were consistent with a NREM parasomnia. In the example below, the patient was shaking her arm – muscle activity (EMG) is shown in the green trace.
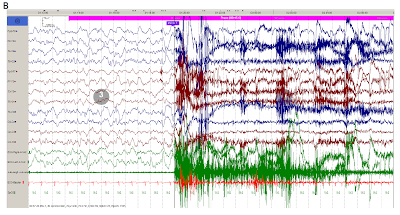 adapted from Fig. 1B (Mantoan et al., 2013). EEG showing delta waves of stage 3 sleep before an episode of arousal with shaking of one arm and looks of fear. Channels 1-12 are EEG; channels 13 and 14 are electro-oculogram (EOG) activity; channel 15 is electromyography (EMG); channel 16 is electrocardiogram (ECG); channel 17 is oxygen saturation by pulse oximetry (SpO2). {click on image for a larger view}
adapted from Fig. 1B (Mantoan et al., 2013). EEG showing delta waves of stage 3 sleep before an episode of arousal with shaking of one arm and looks of fear. Channels 1-12 are EEG; channels 13 and 14 are electro-oculogram (EOG) activity; channel 15 is electromyography (EMG); channel 16 is electrocardiogram (ECG); channel 17 is oxygen saturation by pulse oximetry (SpO2). {click on image for a larger view}
What did the doctors do to help this poor woman? Nothing, it seems. A few more musculoskeletal causes need to be ruled out.
The authors end on a vague note about the possible mechanism(s):
So instead of the more typical visual hallucinations, the patient experiences pain hallucinations that originate.... where?? It seems to me that the sleep EEG could be analyzed more thoroughly, beyond merely ruling out seizure occurrence. Perhaps another imaging modality like PET could be tried (PET would be quieter than fMRI and would better tolerate movement). Identifying the neurophysiological correlates of her phantom night terror pain would provide a fascinating glimpse into a highly unusual sensory phenomenon.2
Further Reading
The Phenomenology of Pain During REM Sleep
The Neurophysiology of Pain During REM Sleep
Footnotes
1 The questions asked in the telephone interviews by Ohayon et al. (1996) were:
2 I've occasionally felt pain in dreams that vanished upon awakening, but I'm pretty sure the episodes occurred during REM (or another stage of dreaming sleep), because visual narrative content was associated with the episodes. Those experiences were clearly not night terrors, and very different from what was reported in the case study.
References
Mantoan L, Eriksson SH, Nisbet AP, & Walker MC (2013). Adult-onset NREM parasomnia with hypnopompic hallucinatory pain: a case report. Sleep, 36 (2), 287-90 PMID: 23372277
Ohayon MM, Priest RG, Caulet M, & Guilleminault C (1996). Hypnagogic and hypnopompic hallucinations: pathological phenomena? The British journal of psychiatry, 169 (4), 459-67 PMID: 8894197
Pigeon WR, Campbell CE, Possemato K, Ouimette P. (2013). Longitudinal relationships of insomnia, nightmares, and PTSD severity in recent combat veterans. J Psychosom Res. 75:546-50.
The Sleep Paralysis Project
- Not Such A Bad Night's Sleep
From 'The Archives', first published in the Digest 2/2/2004 For the 33 percent of Americans who suffer from insomnia, a good night's sleep is no more than a dream. Part of the their problem could be that they overestimate how long it takes...
- You're Feeling Very Sleepy
Just thinking that they’ve not had much sleep could interfere with the daytime functioning of imsomniacs, regardless of whether they actually had enough sleep or not. Twenty-two students (average age 21 years) with primary insomnia were recruited by...
- The Phenomenology Of Pain During Rem Sleep
Coarse — Pain in Dreams Have you ever felt pain in dreams? I have. Once I dreamed I was lying on my stomach, getting a tattoo on my calf against my will. Because it was a particularly malevolent tattoo studio, I cried out in the dream. When I woke up,...
- To Die, To Sleep;
To sleep: perchance to dream: ay, there's the rub; For in that sleep of death what dreams may come When we have shuffled off this mortal coil, Must give us pause... -- William Shakespeare - To be, or not to be (from Hamlet 3/1) Jacob's Dream woodcut,...
- Fda: Insomnia Drug Approval
From the FDA: For Immediate Release: Nov. 23, 2011 FDA approves first insomnia drug for middle-of-the-night waking followed by difficulty returning to sleep [snippet] The U.S. Food and Drug Administration today approved Intermezzo (zolpidem tartrate sublingual...
Neuroscience
When Waking Up Becomes the Nightmare: Hypnopompic Hallucinatory Pain
Most of us have had frightening nightmares – someone is chasing after us trying to kill us, or the world is coming to an end. Other disturbing dreams are based on real life anxieties – our partner leaves us, we lose our job, we become homeless. One specific psychiatric condition includes nightmares as part of the diagnosis. Individuals with post-traumatic stress disorder (PTSD) often have terrible nightmares that relive the traumatic event (Pigeon et al., 2013)
We're always glad to wake up from such nightmares, whether they were of the supernatural or mundane or terrifying variety. "Thank god it was only a dream," we say.
But what if waking up from sleep was the nightmare? Hypnopompic hallucinations are unusual sensory phenomena experienced just before or during awakening. Their better known mirror image, hypnagogic hallucinations, are vivid and frightening episodes of seeing or hearing or feeling phantom sensations while falling asleep (or in early stage 1 sleep). Both are frequently associated with sleep paralysis, the terrifying condition of being half awake but unable to move. This is because the complete muscle atonia typically experienced during REM sleep has oozed into lighter stages of non-REM sleep.

Hypnagogic and hypnopompic hallucinations are usually associated with narcolepsy, but 37% of a representative community sample reported frequent hypnagogic hallucinations, and 12.5% reported hypnopompic hallucinations (Ohayon et al., 1996).1 This went well beyond the low incidence of narcolepsy in that population. Both types of hallucinations were more common in those with insomnia, excessive daytime sleepiness, anxiety disorders, and depression (according to self-report).

Night Terrors 1, by Beth Robinson
Nocturnal Episodes of Pain and Screaming
A new case study in the journal Sleep (Mantoan et al., 2013) reports on the terrifying hypnopompic hallucinations of a 43 year old woman who experiences intense limb pain when waking up, which vanishes within 30 seconds. This is a very unusual manifestation of a non-REM parasomnia, a sleep disorder involving partial arousal during the transition between non-REM and wakefulness. The phenomenology might be best characterized as a night terror.
According to the case report (Mantoan et al., 2013), the patient had...
...a history of nocturnal screaming episodes within 1–2 h of sleep onset from the age of 30 years. Her husband was habitually awoken by his wife screaming loudly, usually flapping either her right or left hand against the bed in a semi-purposeful fashion. Her husband reported that the events were sometimes heralded by an inspiratory sigh, she looked terrified and would not respond to him. The screaming would usually last 5–10 sec, and she would then complain to her husband of intense pain affecting the fingers of either hand or arm and occasionally her legs, with no associated numbness or paraesthesia. She would become fully orientated within 30 sec and would be partially amnesic for the event, but would recall an accompanying sense of “fighting to stay alive” associated with intense panic and often accompanied by fast regular palpitations. Otherwise no dream mentation or visualizations were reported in association with the episodes.
She initially had these episodes monthly, but they increased in frequency to 2-5 times a week with 1-2 episodes per night.
She was unable to identify any triggers for the episodes, and neither she nor her husband considered her to be stressed, anxious, or depressed. There was no history of sleep violence, sleep sex, sleep eating, or any other NREM parasomniac automatisms.
The authors could not identify any standard physical source for the pain. Thoracic outlet syndrome, cervical radiculopathy, focal nerve entrapment, and median neuropathy (carpal tunnel syndrome) were all ruled out.
Pharmacological treatments were unsuccessful. A low dose (0.5–1 mg) of clonazepam was poorly tolerated (it made her feel depressed) and had no effect on her symptoms. Paroxetine was poorly tolerated (due to sedative effects), and gabapentin was also a complete failure. Trazodone, a sedating antidepressant most often prescribed for insomnia, actually made the symptoms worse.
An MRI ruled out a thalamic or hypothalamic lesion. Sleep EEG revealed sudden arousals from deep sleep, accompanied by looks of pain and/or fear on the patient's face. The episodes were consistent with a NREM parasomnia. In the example below, the patient was shaking her arm – muscle activity (EMG) is shown in the green trace.
What did the doctors do to help this poor woman? Nothing, it seems. A few more musculoskeletal causes need to be ruled out.
The authors end on a vague note about the possible mechanism(s):
In conclusion, to our knowledge this is the first report of a NREM parasomnia associated with painful paroxysms, for which we postulate the following underlying pathophysiological mechanism: an internal or external stimulus triggers arousal, facilitating the activation of innate motor pattern generators in the brainstem and activating somatosensory cortical areas to produce hypnopompic hallucinatory pain.
So instead of the more typical visual hallucinations, the patient experiences pain hallucinations that originate.... where?? It seems to me that the sleep EEG could be analyzed more thoroughly, beyond merely ruling out seizure occurrence. Perhaps another imaging modality like PET could be tried (PET would be quieter than fMRI and would better tolerate movement). Identifying the neurophysiological correlates of her phantom night terror pain would provide a fascinating glimpse into a highly unusual sensory phenomenon.2
Further Reading
The Phenomenology of Pain During REM Sleep
The Neurophysiology of Pain During REM Sleep
Footnotes
1 The questions asked in the telephone interviews by Ohayon et al. (1996) were:
(a) Do you experience at least twice a week the following perceptions?To me, the most surprising part of the survey is that 37% reported these phenomenon at sleep onset twice a week for the past year. This contrasts sharply with only 0.04% reporting symptoms of narcolepsy.
(i) the realistic feeling that someone or something is present in the room
(ii) a vivid experience of being caught in a fire
(iii) a vivid experience that you are about to be attacked
(iv) a vivid experience that you are flying through the air
(v) the feeling that you will soon fall into an abyss
(vi) the feeling that shadows or objects are moving and distorting.
(b) Do you experience other types of vivid perceptions?
(c) Can you specify the type of perception?
(i) auditory
(ii) visual
(iii) kinetic (involving movement)
2 I've occasionally felt pain in dreams that vanished upon awakening, but I'm pretty sure the episodes occurred during REM (or another stage of dreaming sleep), because visual narrative content was associated with the episodes. Those experiences were clearly not night terrors, and very different from what was reported in the case study.
References
Mantoan L, Eriksson SH, Nisbet AP, & Walker MC (2013). Adult-onset NREM parasomnia with hypnopompic hallucinatory pain: a case report. Sleep, 36 (2), 287-90 PMID: 23372277
Ohayon MM, Priest RG, Caulet M, & Guilleminault C (1996). Hypnagogic and hypnopompic hallucinations: pathological phenomena? The British journal of psychiatry, 169 (4), 459-67 PMID: 8894197
Pigeon WR, Campbell CE, Possemato K, Ouimette P. (2013). Longitudinal relationships of insomnia, nightmares, and PTSD severity in recent combat veterans. J Psychosom Res. 75:546-50.
The Sleep Paralysis Project
- Not Such A Bad Night's Sleep
From 'The Archives', first published in the Digest 2/2/2004 For the 33 percent of Americans who suffer from insomnia, a good night's sleep is no more than a dream. Part of the their problem could be that they overestimate how long it takes...
- You're Feeling Very Sleepy
Just thinking that they’ve not had much sleep could interfere with the daytime functioning of imsomniacs, regardless of whether they actually had enough sleep or not. Twenty-two students (average age 21 years) with primary insomnia were recruited by...
- The Phenomenology Of Pain During Rem Sleep
Coarse — Pain in Dreams Have you ever felt pain in dreams? I have. Once I dreamed I was lying on my stomach, getting a tattoo on my calf against my will. Because it was a particularly malevolent tattoo studio, I cried out in the dream. When I woke up,...
- To Die, To Sleep;
To sleep: perchance to dream: ay, there's the rub; For in that sleep of death what dreams may come When we have shuffled off this mortal coil, Must give us pause... -- William Shakespeare - To be, or not to be (from Hamlet 3/1) Jacob's Dream woodcut,...
- Fda: Insomnia Drug Approval
From the FDA: For Immediate Release: Nov. 23, 2011 FDA approves first insomnia drug for middle-of-the-night waking followed by difficulty returning to sleep [snippet] The U.S. Food and Drug Administration today approved Intermezzo (zolpidem tartrate sublingual...
