Neuroscience
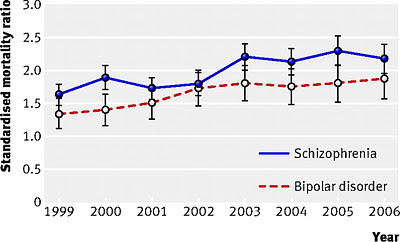 Fig 1 (Hoang et al., 2011). Trend in standardised 365 day all cause mortality ratio for all people discharged from hospital with principal diagnosis of bipolar disorder or schizophrenia.
Fig 1 (Hoang et al., 2011). Trend in standardised 365 day all cause mortality ratio for all people discharged from hospital with principal diagnosis of bipolar disorder or schizophrenia.
The "mortality gap" is the differential between the mortality rates for the general population and for persons with serious mental illness (schizophrenia and bipolar disorder). A new study from England examined hospital records for psychiatric patients discharged between 1999 and 2006, and determined how many had died within one year (Hoang et al., 2011). The authors expected to see a drop in the mortality gap over time due to government programs:
These concerns were mentioned earlier in a systematic review of the literature by Saha et al. (2007), who urged immediate action:
References
Chang CK, Hayes RD, Perera G, Broadbent MT, Fernandes AC, Lee WE, Hotopf M, Stewart R. (2011). Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS ONE 6(5):e19590.
Hoang, U., Stewart, R., & Goldacre, M. (2011). Mortality after hospital discharge for people with schizophrenia or bipolar disorder: retrospective study of linked English hospital episode statistics, 1999-2006. BMJ, 343:d5422. DOI: 10.1136/bmj.d5422
Daumit GL, Dalcin AT, Jerome GJ, Young DR, Charleston J, Crum RM, Anthony C, Hayes JH, McCarron PB, Khaykin E, Appel LJ. (2010). A behavioral weight-loss intervention for persons with serious mental illness in psychiatric rehabilitation centers. Int J Obes (Lond). 35(8):1114-23.
Saha S, Chant D, McGrath J (2007). A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry 64:1123-31.
October 10 was World Mental Health Day, an event designed to raise public awareness of mental health issues:
- Can Pot Smoking Counter The Negative Metabolic Consequences Of Atypical Antipsychotics?
DISCLAIMER: This is a hypothetical question and not a medical recommendation. But it might be an idea worth investigating in epidemiological studies. Everyone knows that pot gives you the munchies. So the paradoxical finding that marijuana use is associated...
- Fda: Saphris (asenapine) Approval, Schizophrenia And Bipolar
From the FDA: FDA Approves Saphris to Treat Schizophrenia and Bipolar Disorder The U.S. Food and Drug Administration has approved Saphris tablets (asenapine) to treat adults with schizophrenia, a chronic, severe and disabling brain disorder, and to treat...
- Neuropsychology Abstract Of The Day: Cognitive Function In 95-year-olds
Börjesson-Hanson A, Gustafson D, & Skoog I. Five-year mortality in relation to dementia and cognitive function in 95-year-olds. Neurology. 2007 Nov 27; 69(22): 2069-2075. Neuropsychiatric Epidemiology Unit, Psychiatry Section, Institute of Neuroscience...
- Risperdal (risperidone) And Pediatric Schizophrenia And Bipolar Disorder
An FDA press release from yesterday: FDA Approves Risperdal for Two Psychiatric Conditions in Children and Adolescents The U.S. Food and Drug Administration today approved Risperdal (risperidone) for the treatment of schizophrenia in adolescents, ages...
- Johns Hopkins Master Of Health Science In Mental Health Degree!
The Johns Hopkins Bloomberg School of Public Health, Department of Mental Health invites applications for the Master of Health Science degree program for the 2016/2017 academic year (due June 1, 2016). https://drive.google.com/file/d/0B-WK1jWUo8h2YTNZUzZRSGdjM28/view?usp=sharing...
Neuroscience
Rising Mortality Rates for People with Serious Mental Illness
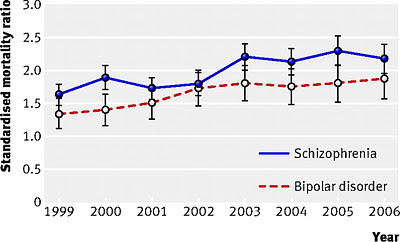 Fig 1 (Hoang et al., 2011). Trend in standardised 365 day all cause mortality ratio for all people discharged from hospital with principal diagnosis of bipolar disorder or schizophrenia.
Fig 1 (Hoang et al., 2011). Trend in standardised 365 day all cause mortality ratio for all people discharged from hospital with principal diagnosis of bipolar disorder or schizophrenia.The "mortality gap" is the differential between the mortality rates for the general population and for persons with serious mental illness (schizophrenia and bipolar disorder). A new study from England examined hospital records for psychiatric patients discharged between 1999 and 2006, and determined how many had died within one year (Hoang et al., 2011). The authors expected to see a drop in the mortality gap over time due to government programs:
Over the past decade several strategies have been implemented in England and Wales aimed at reducing the mortality gap between people with serious mental illness and the general population, including those to address deliberate self harm and to reduce suicide (7 8 9), to decrease smoking (10 11 12), alcoholism, and drug misuse (13 14) and to deal with other lifestyles associated with increased mortality (15 16). Recent studies have suggested that the rate of suicide has been stabilising among people with mental disorders as a whole (17 18 19 20 21); however, trends in mortality for people with schizophrenia or bipolar disorder remain poorly characterised, particularly the relative contributions of natural and unnatural causes. The United Kingdom government’s recent mental health strategy states that “more people with mental health problems will have good physical health” as one of its objectives, specifically stating that “fewer people with mental health problems will die prematurely” (22). It is therefore timely to review the level of and trends in these recognised inequalities.However, as illustrated in Fig. 1 above, the opposite trend was observed, with increased mortality for those with schizophrenia and bipolar disorder. The standardized mortality ratios show a rise from ~30-60% greater than the general population to about double the population average:
For people discharged with schizophrenia, the ratio was 1.6 in 1999 and 2.2 in 2006 (P<0.001 for trend). For bipolar disorder, the ratios were 1.3 in 1999 and 1.9 in 2006 (P=0.06 for trend). Ratios were higher for unnatural than for natural causes. About three quarters of all deaths, however, were certified as natural, and increases in ratios for natural causes, especially circulatory disease and respiratory diseases, were the main components of the increase in all cause mortality.These results are alarming (but not new, unfortunately) and similar to those reported by Chang et al. (2011) - see Improving the Physical Health of People With Serious Mental Illness. In that post, I mentioned the possible role of "second generation" or atypical antipsychotics, which can cause substantial weight gain and hence diabetes, hypertension, cardiovascular problems, high cholesterol, and stroke. To counteract these serious side effects, a regular part of mental health treatment should include programs that promote better physical health: smoking cessation and nutritionists and structured exercise classes in addition to standard psychiatric care and substance abuse treatment. For example, a six month intervention pilot study enrolled 63 overweight participants at psychiatric rehabilitation day programs and showed promising initial results (Daumit et al., 2010).
These concerns were mentioned earlier in a systematic review of the literature by Saha et al. (2007), who urged immediate action:
“in light of the potential for second-generation antipsychotic medications to further adversely influence mortality rates . . . optimizing the general health of people with schizophrenia warrants urgent attention.”
References
Chang CK, Hayes RD, Perera G, Broadbent MT, Fernandes AC, Lee WE, Hotopf M, Stewart R. (2011). Life expectancy at birth for people with serious mental illness and other major disorders from a secondary mental health care case register in London. PLoS ONE 6(5):e19590.
Hoang, U., Stewart, R., & Goldacre, M. (2011). Mortality after hospital discharge for people with schizophrenia or bipolar disorder: retrospective study of linked English hospital episode statistics, 1999-2006. BMJ, 343:d5422. DOI: 10.1136/bmj.d5422
Daumit GL, Dalcin AT, Jerome GJ, Young DR, Charleston J, Crum RM, Anthony C, Hayes JH, McCarron PB, Khaykin E, Appel LJ. (2010). A behavioral weight-loss intervention for persons with serious mental illness in psychiatric rehabilitation centers. Int J Obes (Lond). 35(8):1114-23.
Saha S, Chant D, McGrath J (2007). A systematic review of mortality in schizophrenia: is the differential mortality gap worsening over time? Arch Gen Psychiatry 64:1123-31.
~~~~~~~~~~~
October 10 was World Mental Health Day, an event designed to raise public awareness of mental health issues:
This year the theme is "Investing in mental health". Financial and human resources allocated for mental health are inadequate especially in low resource countries. The majority of low- and middle-income countries spend less than 2% of their health budget on mental health. Many countries have less than one mental health specialist per one million population. Even a considerable part of the limited resources is spent on large mental hospitals and not for services delivered through community and primary health care.We need to increase investment for mental health and to shift the available resources towards more effective and more humanitarian forms of services.More information and links available at Providentia and The Amazing World of Psychiatry.
World Mental Health Day Blog Party, sponsored by Psych Central.
- Can Pot Smoking Counter The Negative Metabolic Consequences Of Atypical Antipsychotics?
DISCLAIMER: This is a hypothetical question and not a medical recommendation. But it might be an idea worth investigating in epidemiological studies. Everyone knows that pot gives you the munchies. So the paradoxical finding that marijuana use is associated...
- Fda: Saphris (asenapine) Approval, Schizophrenia And Bipolar
From the FDA: FDA Approves Saphris to Treat Schizophrenia and Bipolar Disorder The U.S. Food and Drug Administration has approved Saphris tablets (asenapine) to treat adults with schizophrenia, a chronic, severe and disabling brain disorder, and to treat...
- Neuropsychology Abstract Of The Day: Cognitive Function In 95-year-olds
Börjesson-Hanson A, Gustafson D, & Skoog I. Five-year mortality in relation to dementia and cognitive function in 95-year-olds. Neurology. 2007 Nov 27; 69(22): 2069-2075. Neuropsychiatric Epidemiology Unit, Psychiatry Section, Institute of Neuroscience...
- Risperdal (risperidone) And Pediatric Schizophrenia And Bipolar Disorder
An FDA press release from yesterday: FDA Approves Risperdal for Two Psychiatric Conditions in Children and Adolescents The U.S. Food and Drug Administration today approved Risperdal (risperidone) for the treatment of schizophrenia in adolescents, ages...
- Johns Hopkins Master Of Health Science In Mental Health Degree!
The Johns Hopkins Bloomberg School of Public Health, Department of Mental Health invites applications for the Master of Health Science degree program for the 2016/2017 academic year (due June 1, 2016). https://drive.google.com/file/d/0B-WK1jWUo8h2YTNZUzZRSGdjM28/view?usp=sharing...
