Neuroscience
When I critiqued Morrison et als exploratory CBT trial with people who stop taking anti-psychotic medication, I promised to write a post on the final study
Well it appeared in the Lancet today and a free copy is here. I am not going to describe the study in detail as it is excellently covered in the Mental Elf blog today. Contrary to the fanfare of glowing comments by highly respected schizophrenia/psychosis researchers, I think the paper has so many issues that I may need to write a second post. But I'm keeping it simple here to concentrate on the primary outcome data - symptom change scores on the PANSS.
The study examines schizophrenia patients who have decided not to take anti-psychotic medications; 37 were randomly assigned to 9 months CBT and 37 assigned to - what the authors call TAU (but is obviously quite unusual...in an important manner that will become clear below)
What do the primary outcome PANSS scores (total, positive and negative symptoms) reveal?
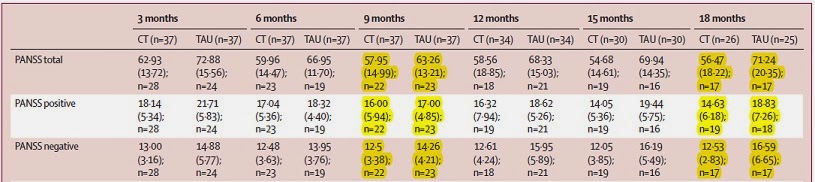
Table 1. PANSS scores during the intervention (up to 9 months) and follow ups to 18 months
The key questions are:
Do the CBT and TAU groups differ in PANSS scores at the end of the intervention (9 months) and at the end of the study (18 months)? One simple way to address both questions is to calculate the Effect Sizes at 9 months and at 18 months.
9 months
A closer inspection of the means shows that the significant differences at 18 months almost certainly reflects an increase in symptom scores for the TAU group rather than a decrease for the CBT group (compare CBT at 9 and 18 months and TAU at 9 and 18 months)
My final and crucial point concerns within group symptom reduction
Table 2 shows the baseline PANSS scores on primary outcome measures and its informative to compare change from baseline within each group (CBT and control)
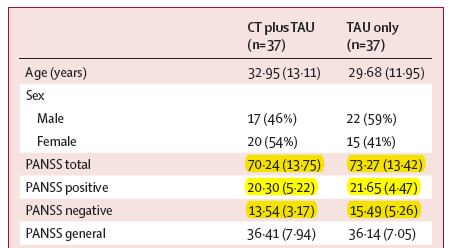
If we compare baseline and the end of the intervention 9 months:
PANSS total
CBT group show a reduction from 70.24 to 57.95 =12.29
TAU group show a reduction from 73.27 to 63.26 =10.01
PANSS positive
CBT group show a reduction from 20.30 to 16.0 =4.30
TAU group show a reduction from 21.65 to 17.0 = 4.65
PANSS negative
CBT group show a reduction from 13.54 to 12.50 = 1.04
TAU group show a reduction from 15.49 to 14.26 = 1.23
So, after 9 months of intensive CBT intervention, controls - who don't even receive a placebo - show a greater reduction in positive and negative symptoms !
Moreover, the 'natural' reduction shown at 9 months by TAU is as large as the reduction shown by the CBT group at the very end of the trial (18 months: PANSS total =13.77; PANSS pos 5.67 and PANSS neg 1.01) - no significant difference exists between TAU reduction at 9 months and CBT reduction at 9 or 18 months
What then have Morrison et al shown?
I would argue that their data show, for the first time, how patients who choose to be unmedicated display fluctuations in symptomatology (as we might expect given they are unmedicated) ...but crucially, these fluctuations are as large as the changes seen in the CBT group. Hence, it is reasonable to ask...have Morrison et al simply documented 'normal fluctuation' in the symptomatology of unmedicated patients ...and nothing to do with CBT
- Neuropsychology Abstract Of The Day: Ms And Cognitive Rehabilitation
A randomized controlled trial of a cognitive rehabilitation intervention for persons with multiple sclerosis Clin Rehabil. 2012 Feb 2; Stuifbergen AK, Becker H, Perez F, Morison J, Kullberg V, Todd A Abstract Objective: To explore the feasibility and...
- Neuropsychology Abstract Of The Day: Cognitive Intervention In Amnestic Mci And Mild Alzheimer's Disease
Effects of a 6-Month Cognitive Intervention on Brain Metabolism in Patients with Amnestic MCI and Mild Alzheimer's Disease. Journal of Alzheimers Disease. 2011 Jan 1;26(0):337-48 Authors: Förster S, Buschert VC, Teipel SJ, Friese U, Buchholz HG,...
- Neuropsychology Abstract Of The Day: Donepezil And Aphasia
Chen Y, Li YS, Wang ZY, Xu Q, Shi GW, & Lin Y. [The efficacy of donepezil for post-stroke aphasia: a pilot case control study.] Zhonghua Nei Ke Za Zhi. 2010 Feb, 49(2), 115-118. OBJECTIVE: To evaluate the efficacy of donepezil for post-stroke aphasia....
- Significantly Nonsignificant
In the morning I'd awake and I couldn't remember What is love and what is hate? - the calculations error Flaming Lips (Morning of the Magicians) Cognitive behaviour therapy for psychosis can be adapted for minority ethnic groups: A randomised...
- Cbt: You Spin Me Round
Although we failed to show a statistically significant effect of the intervention we cannot rule out a beneficial effect of the cognitive therapy on transition rate (although it could be argued that the sample size required to show such an effect,...
Neuroscience
My Bloody Valentine: CBT for unmedicated psychosis
When I critiqued Morrison et als exploratory CBT trial with people who stop taking anti-psychotic medication, I promised to write a post on the final study
Well it appeared in the Lancet today and a free copy is here. I am not going to describe the study in detail as it is excellently covered in the Mental Elf blog today. Contrary to the fanfare of glowing comments by highly respected schizophrenia/psychosis researchers, I think the paper has so many issues that I may need to write a second post. But I'm keeping it simple here to concentrate on the primary outcome data - symptom change scores on the PANSS.
'Soon' by My Bloody Valentine (Andy Weatherall mix)
The study examines schizophrenia patients who have decided not to take anti-psychotic medications; 37 were randomly assigned to 9 months CBT and 37 assigned to - what the authors call TAU (but is obviously quite unusual...in an important manner that will become clear below)
What do the primary outcome PANSS scores (total, positive and negative symptoms) reveal?
Table 1. PANSS scores during the intervention (up to 9 months) and follow ups to 18 months
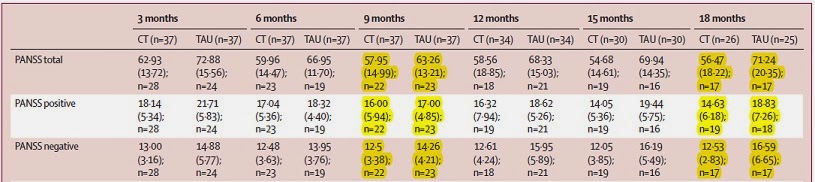
The key questions are:
Do the CBT and TAU groups differ in PANSS scores at the end of the intervention (9 months) and at the end of the study (18 months)? One simple way to address both questions is to calculate the Effect Sizes at 9 months and at 18 months.
9 months
PANSS total = -0.37 (95 CI -0.96 to 0.22)
PANSS positive = -0.18 (95 CI -0.77 to 0.40)
PANSS negative = -0.45 (95 CI -1.04 to 0.14)
Examination of effect sizes at the end of the intervention (9 months) reveals that CBT and TAU groups do not differ significantly on any of the three primary outcome measures at the end of intervention (i.e. all CIs cross zero)
18 monthsPANSS positive is nonsignificant, while PANSS total and PANSS negative effect sizes are moderately sized, the lower end CIs are very close to zero (at -0.05 and -0.08) suggesting marginal significance
18 months
PANSS total = -0.75 (95 CI -1.44 to -0.05)
PANSS positive = -0.61 (95 CI -1.27 to 0.05)
PANSS negative = -0.45 (95 CI -1.47 to -0.08)
A closer inspection of the means shows that the significant differences at 18 months almost certainly reflects an increase in symptom scores for the TAU group rather than a decrease for the CBT group (compare CBT at 9 and 18 months and TAU at 9 and 18 months)
My final and crucial point concerns within group symptom reduction
Table 2 shows the baseline PANSS scores on primary outcome measures and its informative to compare change from baseline within each group (CBT and control)
Table 2. PANSS scores at baseline
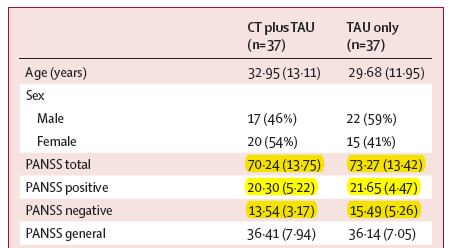
If we compare baseline and the end of the intervention 9 months:
PANSS total
CBT group show a reduction from 70.24 to 57.95 =12.29
TAU group show a reduction from 73.27 to 63.26 =10.01
PANSS positive
CBT group show a reduction from 20.30 to 16.0 =4.30
TAU group show a reduction from 21.65 to 17.0 = 4.65
PANSS negative
CBT group show a reduction from 13.54 to 12.50 = 1.04
TAU group show a reduction from 15.49 to 14.26 = 1.23
So, after 9 months of intensive CBT intervention, controls - who don't even receive a placebo - show a greater reduction in positive and negative symptoms !
Moreover, the 'natural' reduction shown at 9 months by TAU is as large as the reduction shown by the CBT group at the very end of the trial (18 months: PANSS total =13.77; PANSS pos 5.67 and PANSS neg 1.01) - no significant difference exists between TAU reduction at 9 months and CBT reduction at 9 or 18 months
What then have Morrison et al shown?
I would argue that their data show, for the first time, how patients who choose to be unmedicated display fluctuations in symptomatology (as we might expect given they are unmedicated) ...but crucially, these fluctuations are as large as the changes seen in the CBT group. Hence, it is reasonable to ask...have Morrison et al simply documented 'normal fluctuation' in the symptomatology of unmedicated patients ...and nothing to do with CBT
- Neuropsychology Abstract Of The Day: Ms And Cognitive Rehabilitation
A randomized controlled trial of a cognitive rehabilitation intervention for persons with multiple sclerosis Clin Rehabil. 2012 Feb 2; Stuifbergen AK, Becker H, Perez F, Morison J, Kullberg V, Todd A Abstract Objective: To explore the feasibility and...
- Neuropsychology Abstract Of The Day: Cognitive Intervention In Amnestic Mci And Mild Alzheimer's Disease
Effects of a 6-Month Cognitive Intervention on Brain Metabolism in Patients with Amnestic MCI and Mild Alzheimer's Disease. Journal of Alzheimers Disease. 2011 Jan 1;26(0):337-48 Authors: Förster S, Buschert VC, Teipel SJ, Friese U, Buchholz HG,...
- Neuropsychology Abstract Of The Day: Donepezil And Aphasia
Chen Y, Li YS, Wang ZY, Xu Q, Shi GW, & Lin Y. [The efficacy of donepezil for post-stroke aphasia: a pilot case control study.] Zhonghua Nei Ke Za Zhi. 2010 Feb, 49(2), 115-118. OBJECTIVE: To evaluate the efficacy of donepezil for post-stroke aphasia....
- Significantly Nonsignificant
In the morning I'd awake and I couldn't remember What is love and what is hate? - the calculations error Flaming Lips (Morning of the Magicians) Cognitive behaviour therapy for psychosis can be adapted for minority ethnic groups: A randomised...
- Cbt: You Spin Me Round
Although we failed to show a statistically significant effect of the intervention we cannot rule out a beneficial effect of the cognitive therapy on transition rate (although it could be argued that the sample size required to show such an effect,...
