Neuroscience
Are you having trouble sleeping? But you're not feeling that 19th century retro hipster insomniac vibe? Try some of these behavioral remedies recommended by the finest scientific and medical journals of today.

What a Difference a Day Makes
Is Intensive Sleep Retraining (ISR) a new overnight treatment for chronic insomnia (Harris et al., 2012)? ISR is conducted in one 25 hr session at a sleep lab, where the insomniac sleeps a maximum of 3 min every 30 min for a period of 25 hrs. Instant cure! (supposedly). The basic idea is that the person will learn they can fall asleep fairly quickly and easily, and this will translate directly to real life sleeping patterns.
In a commentary accompanying the main article in Sleep, Spielman and Glovinsky (2012) describe it as:
The highly intrusive ISR procedure involved arriving at 21:00.
Ultimately, did this punitive procedure work? Yes. But it wasn't significantly better than SCT for most of the subjective sleep measures used. All three active treatment conditions produced improvements in self-reported duration and efficiency of sleep, relative to the SH control. Of the 16 or so analyses at 2 of 7 selected time points (which did not seem to be corrected for multiple comparisons), there were some instances where ISR or the combined ISR + SCT treatment was better than stimulus control therapy (see below), but nothing earth shattering.
In another graph (Fig. 5 - Mean sleep diary wake time after sleep onset), the SCT groups were superior to ISR at Week 1 and Post-Treatment.
What about the objective sleep measures obtained by actigraphy?
So what's next? Intensive Sleep Retraining is costly and available only from highly specialized centers.1 But the possibility of self-administered ISR is on the horizon, using portable EEG headsets, actigraphs, and vibrating alarms. Is there an app for that?

Footnote
1 I'm not sure that it's even being offered as a clinical treatment. The RCT was conducted in Australia.
References
Harris, J., Lack, L., Kemp, K., Wright, H., & Bootzin, R. (2012). A Randomized Controlled Trial of Intensive Sleep Retraining (ISR): A Brief Conditioning Treatment for Chronic Insomnia. SLEEP DOI: 10.5665/sleep.1584
Spielman, A., & Glovinsky, P. (2012). What a Difference a Day Makes. SLEEP DOI: 10.5665/sleep.1574

In case you're interested in learning more about 19th century scientific views and treatments for insomnia, see these books, which are online in their entirety:
L'insomnie et son traitement / by Maurice de Fleury (1894)Sleep and sleeplessness / by J. Mortimer-Granville (1881)Sleep, insomnia, and hypnotics / by Edward Payson Hurd (1891)
- Students: It's Time To Ditch The Pre-exam All-nighter
Lack of sleep impairs the human brain's ability to store new information in memory, researchers have found. Past research has already shown that sleep is vital for consolidating recently-learned material but now Matthew Walker and colleagues have...
- You're Feeling Very Sleepy
Just thinking that they’ve not had much sleep could interfere with the daytime functioning of imsomniacs, regardless of whether they actually had enough sleep or not. Twenty-two students (average age 21 years) with primary insomnia were recruited by...
- To Die, To Sleep;
To sleep: perchance to dream: ay, there's the rub; For in that sleep of death what dreams may come When we have shuffled off this mortal coil, Must give us pause... -- William Shakespeare - To be, or not to be (from Hamlet 3/1) Jacob's Dream woodcut,...
- Fda: Insomnia Drug Approval
From the FDA: For Immediate Release: Nov. 23, 2011 FDA approves first insomnia drug for middle-of-the-night waking followed by difficulty returning to sleep [snippet] The U.S. Food and Drug Administration today approved Intermezzo (zolpidem tartrate sublingual...
- Sleep Now
["... Now" is a short post of cog sci topics in the news] Last week, the New York Times had several articles on sleep. You can see the list at Bora Zivkovic's A Blog Around the Clock blog: Sleeping with the New York Times. David Corcoran of the New...
Neuroscience
21st Century Treatments for Insomnia
Are you having trouble sleeping? But you're not feeling that 19th century retro hipster insomniac vibe? Try some of these behavioral remedies recommended by the finest scientific and medical journals of today.
What a Difference a Day Makes
Is Intensive Sleep Retraining (ISR) a new overnight treatment for chronic insomnia (Harris et al., 2012)? ISR is conducted in one 25 hr session at a sleep lab, where the insomniac sleeps a maximum of 3 min every 30 min for a period of 25 hrs. Instant cure! (supposedly). The basic idea is that the person will learn they can fall asleep fairly quickly and easily, and this will translate directly to real life sleeping patterns.
In a commentary accompanying the main article in Sleep, Spielman and Glovinsky (2012) describe it as:
...a novel insomnia treatment that while radical in procedure is grounded in learning theory, a long-established conceptual framework for understanding insomnia. ISR combines two familiar components of sleep research—sleep deprivation and the polysomnographic recording of sleep onset—to yield an entirely new therapeutic procedure: repeated practice in falling asleep quickly. Massed practice in achieving sleep is here shown to possess a therapeutic value rivaling that of stimulus control therapy (SCT), that mainstay of behavioral sleep medicine, as well as offering a possible additive effect when administered in conjunction with SCT.ISR employs sleep laboratory technology to measure the speed of sleep onset, limit the duration of sleep, and allow immediate feedback to subjects as to whether objectively recorded sleep has occurred. It typically provides dozens of successful entries to sleep over the course of a single night and day. Then it is over, handing off responsibility for good sleep management to sleep hygiene recommendations.In contrast to ISR, there is already strong research support for stimulus control therapy (SCT), which is designed to:
...reduce the anxiety or conditioned arousal individuals may feel when attempting to go to bed. Specifically, a set of instructions designed to reassociate the bed/bedroom with sleep and to re-establish a consistent sleep schedule are implimented. These include: 1) Going to bed only when sleepy; 2) Getting out of bed when unable to sleep; 3) Using the bed/bedroom only for sleep and sex (i.e., no reading, watching TV, etc); 4) Arising at the same time every morning; and 5) Avoiding naps.One question, then, is whether ISR is better than SCT, an accepted behavioral therapy for insomnia. Eighty participants in the study of Harris et al. were randomized into one of four groups: (1) ISR + sleep hygeine instruction (SH); (2) SCT + SH; (3) ISR + SCT; (4) SH alone, which served as the control condition. All participants kept a sleep diary, answered questionnaires, and wore an actigraph to measure motor activity. Those in the ISR groups slept no more than 5 hrs the night before they came to the lab.
The highly intrusive ISR procedure involved arriving at 21:00.
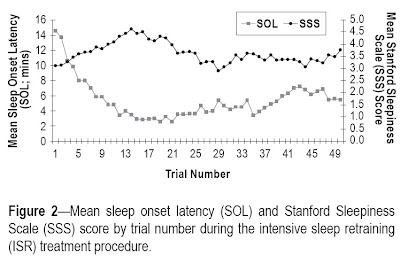
Following an explanation, the signing of an informed consent form, electrode application, and a quiet settling period, treatment began at 22:30. Treatment trials were conducted every half hour, finishing after 23:00 on night 2. Thereby, the ISR treatment routine allowed a series of 50 half-hourly sleep onset opportunities. ... Within each treatment trial, the opportunity for sleep onset was limited to a 20-min period, with the trial stopping if sleep onset had not occurred by this time. For those trials in which sleep was initiated, 3 consecutive minutes of sleep were permitted, prior to being awoken [the method of awakening was not described]. Upon awakening, treatment participants first rated their perception of whether sleep onset had occurred (on a Likert scale of 1 “No, definitely not” to 7 “Yes, definitely”). Following this response, participants were provided with information as to whether sleep onset had or had not occurred.Then they got out of bed to read or watch DVDs. After 10 trials of this nonsense, people were falling asleep in 5 min or less.
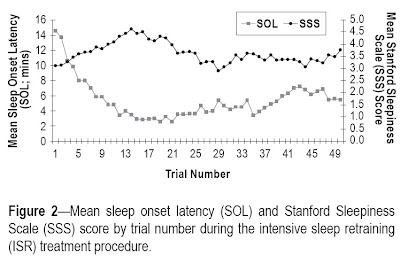
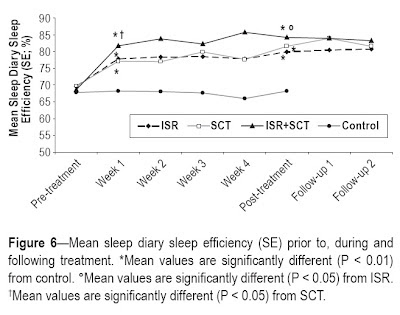
Ultimately, did this punitive procedure work? Yes. But it wasn't significantly better than SCT for most of the subjective sleep measures used. All three active treatment conditions produced improvements in self-reported duration and efficiency of sleep, relative to the SH control. Of the 16 or so analyses at 2 of 7 selected time points (which did not seem to be corrected for multiple comparisons), there were some instances where ISR or the combined ISR + SCT treatment was better than stimulus control therapy (see below), but nothing earth shattering.
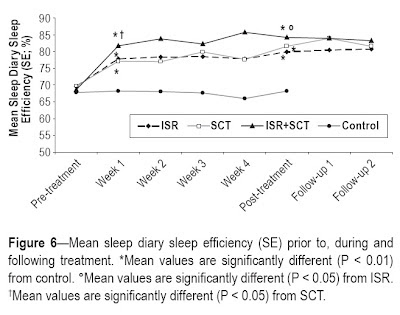
In another graph (Fig. 5 - Mean sleep diary wake time after sleep onset), the SCT groups were superior to ISR at Week 1 and Post-Treatment.
What about the objective sleep measures obtained by actigraphy?
The actigraphy data failed to support significant changes in sleep, despite using an adjusted manual scoring method and a sensitivity setting in the scoring algorithm that calibrated actigraphy TST [total sleep time] to PSG [polysomnography] TST. Actigraphy has similarly failed to mirror subjective sleep changes in other treatment studies in insomnia, and objective measures (i.e., EEG) fail to replicate the extent of subjective sleep changes in clinical insomnia treatment studies.The authors concluded that actigraphy is useless and that subjective sleep report is the only thing that matters (basically).
So what's next? Intensive Sleep Retraining is costly and available only from highly specialized centers.1 But the possibility of self-administered ISR is on the horizon, using portable EEG headsets, actigraphs, and vibrating alarms. Is there an app for that?

Footnote
1 I'm not sure that it's even being offered as a clinical treatment. The RCT was conducted in Australia.
References
Harris, J., Lack, L., Kemp, K., Wright, H., & Bootzin, R. (2012). A Randomized Controlled Trial of Intensive Sleep Retraining (ISR): A Brief Conditioning Treatment for Chronic Insomnia. SLEEP DOI: 10.5665/sleep.1584
Spielman, A., & Glovinsky, P. (2012). What a Difference a Day Makes. SLEEP DOI: 10.5665/sleep.1574

In case you're interested in learning more about 19th century scientific views and treatments for insomnia, see these books, which are online in their entirety:
L'insomnie et son traitement / by Maurice de Fleury (1894)Sleep and sleeplessness / by J. Mortimer-Granville (1881)Sleep, insomnia, and hypnotics / by Edward Payson Hurd (1891)
- Students: It's Time To Ditch The Pre-exam All-nighter
Lack of sleep impairs the human brain's ability to store new information in memory, researchers have found. Past research has already shown that sleep is vital for consolidating recently-learned material but now Matthew Walker and colleagues have...
- You're Feeling Very Sleepy
Just thinking that they’ve not had much sleep could interfere with the daytime functioning of imsomniacs, regardless of whether they actually had enough sleep or not. Twenty-two students (average age 21 years) with primary insomnia were recruited by...
- To Die, To Sleep;
To sleep: perchance to dream: ay, there's the rub; For in that sleep of death what dreams may come When we have shuffled off this mortal coil, Must give us pause... -- William Shakespeare - To be, or not to be (from Hamlet 3/1) Jacob's Dream woodcut,...
- Fda: Insomnia Drug Approval
From the FDA: For Immediate Release: Nov. 23, 2011 FDA approves first insomnia drug for middle-of-the-night waking followed by difficulty returning to sleep [snippet] The U.S. Food and Drug Administration today approved Intermezzo (zolpidem tartrate sublingual...
- Sleep Now
["... Now" is a short post of cog sci topics in the news] Last week, the New York Times had several articles on sleep. You can see the list at Bora Zivkovic's A Blog Around the Clock blog: Sleeping with the New York Times. David Corcoran of the New...
